Cystolitholapaxy
What happens during the procedure?
Either a full general anaesthetic (where you will be asleep throughout the procedure) or a spinal anaesthetic (where you are awake but unable to feel anything from the waist down) will be used. All methods minimise pain; your anaesthetist will explain the pros and cons of each type of anaesthetic to you.
You will usually be given injectable antibiotics before the procedure, after checking for any allergies.
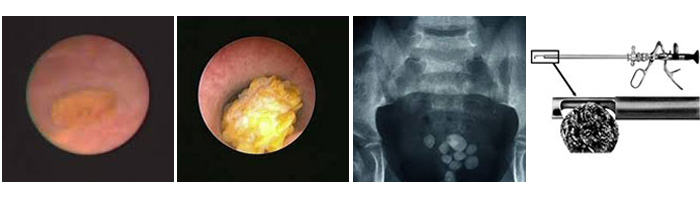
A special telescope is inserted into the bladder to see the stones. These are then broken up using a crushing instrument, a mechanical disintegration probe or a laser. The stone fragments are removed from the bladder and a catheter inserted.
What happens immediately after the procedure?
The catheter will be removed within 24-48 hours following which you will be able to pass urine normally. Some burning, frequency of urination and bleeding are common within the first 24-48 hours after catheter removal.
It is not unusual for a plain X-ray of your abdomen to be performed on the day after surgery to confirm that all the stone fragments have been removed.
The average hospital stay is 2 days.
Are there any side-effects?
Most procedures have a potential for side-effects. You should be reassured that, although all these complications are well-recognised, the majority of patients do not suffer any problems after a urological procedure.
Please use the check boxes to tick off individual items when you are happy that they have been discussed to your satisfaction:
- Mild burning or bleeding on passing urine for short period after operation ¨ Temporary insertion of a catheter ¨ Need for an additional procedure (e.g. resection of the prostate gland) if this is thought to be the cause of the stone formation Cystoscopy & litholapaxy (bladder stone crushing/removal) Page 2 of 6 Occasional (between 1 in 10 and 1 in 50).
- Infection of bladder requiring antibiotics ¨ Permission for telescopic removal/ biopsy of bladder abnormality/stone if found Recurrence of stones or residual stone fragments Rare (less than 1 in 50).
- Delayed bleeding requiring removal of clots or further surgery Injury to the urethra causing delayed scar formation ¨ Very rarely, perforation of the bladder requiring a temporary urinary catheter or return to theatre for open surgical repair Hospital-acquired infection (overall risk for Addenbrooke’s).
- Colonisation with MRSA (0.02%, 1 in 5,000) ¨ Clostridium difficile bowel infection (0.04%; 1 in 2,500) ¨ MRSA bloodstream infection (0.01%; 1 in 10,000) (These rates may be greater in high-risk patients e.g. with long- term drainage tubes, after removal of the bladder for cancer, after previous infections, after prolonged hospitalisation or after multiple admissions).


 WhatsApp Us
WhatsApp Us